Breast Cancer Treatment in Pune
What is Breast cancer?
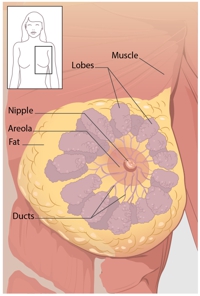
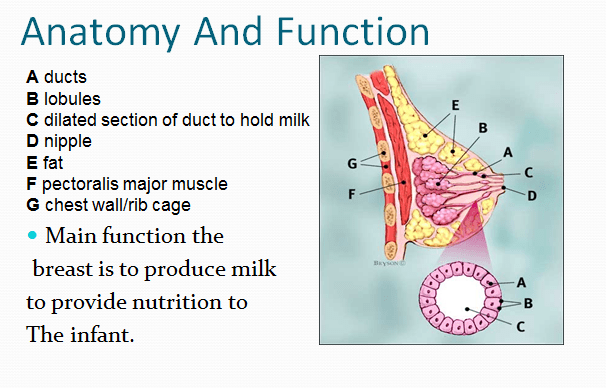
Breast cancer starts from different parts of breast. Commonly it starts in the ducts of breast that carry milk to the nipple. It is also known as ductal cancer. Other type of breast cancer starts in the glands that create breast milk. Lesser no. of cancers start in other breast tissues, sarcomas and lymphomas.
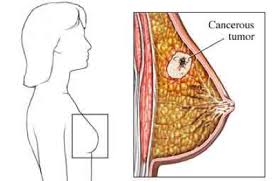
Breast Cancer starts when the cells in the breast start growing out of control. It is the excessive cell growth that causes cancer usually they form a tumour or lump and it can spread to distant parts of the body. Breast cancer commonly starts in the cells of milk ducts (Ductal cell ca ). Sometimes it can start in the glandular cells of the breast (lobular ca ).
Causes Of Breast Cancer :
The exact cause of breast cancer remains unclear but some risk factors make it more likely to happen. Some risk factors are preventable but some are not.
- Gender:
Female gender itself predispose to getting breast cancer. Though very rarely breast cancer can occur in men.
- Age :
The risk increases with age. After an age of 40 yrs, the risk increases steadily so that by the age of 70 yrs it goes up to 3.84 % though breast cancer occur in very young women of early age (20-40) is also becoming common now.
- Family History(Genetics) :
The risk is higher if a woman has or had close relatives with breast cancer such as mother, sister, grandmother.
The risk further increases if the number of relatives is more or if the family member has bilateral breast cancer or breast cancer with Ovarian cancer or a case of male breast cancer in the family.
Women who carry BRCA 1, & BRCA 2 or TPS3 genes have a higher risk of developing breast ca or Ovarian cancer or both.
- A history of Breast Ca or the breast lump :
If a woman had a breast cancer earlier is more likely to get it again either in the same breast or opposite breast compares with the woman having no disease.
Some types of noncancerous(benign) lump increase the chance of developing cancer later on. e.g. Atypical ductal hyperplasia or Lobular cancer insitu -.
- Dense Breast :
Breast cancer is more likely to develop in higher density breast tissue.
- Estrogen Exposure OR Personal History :
Exposure to estrogen for a longer period appears to increase the risk of breast cancer.
- Early menarche (starting period) & late menopause causes the woman to higher exposure to estrogen.
- Late first pregnancy exposes a woman to higher exchange level.
- Breastfeeding especially for over 1 yr appears to reduce the risk probably due to prolonged menstrual cycles.
- Women having we child (melliporous) have higher estrogen exposure & hence higher risk.
- Women taking hormone replacement therapy [HRT] also have higher risk due to estrogen exposure.
- Radiation Exposure :
Exposure to radiation treatment [ e.g. in the patient with lymphomas ] increase the risk of breast cancer later in life.
Symptoms of breast Cancer
Be Breast Aware of symptoms of breast cancer
Breast Cancer can have a number of Symptoms.but for many women it will appear as a lump or thickening in the breast issue.
This may be in the breast itself or upper chest or armpit.
If brest cancer is detected at an early stage, it can be treated before it spreads to other parts of the body.
The earlier the breast cancer is detected, the better the chance of beating it.
Make sure you are breast aware and check your breast regularly. If you know how your breast usually look and feel it will be easier to spot any unusual changes.
What to look for…
- Lump of thickening in the breast tissue
[Although all lumps in the breast are not cancer] - Swelling, Thickening of all or part of breast
(Orange peel Texture.) - Dimpled or depressed skin [in drawn skin]
- Nipple retraction[in drawn nipple]
- Asymmetry of breast/nipple
- Deviation of nipple
- Redness / swelling with lump in the breast
- Ulcer over breast lump
- blood nipple discharge
- Ulceration … over nipple / breast
Risk Factors :
Preventable Risk Factors –
1. Obesity :
Women who are overweight or have obesity after menopause may have higher risk of developing breast cancer possibly due to higher level of estrogen.
2. Physical Activity (Exercise) :
Regular physical activity reduces breast cancer risk, especially in women past menopause. Recommended is 150 min of moderate intensity or 15 min of vigorous intensity activity each week (or a combination of there) spread throughout the week activities like the brisk walk, stretching, weight lifting or yoga are beneficial.
3. Not having children :
Women who do not have children or had their first child after age 30 have a slightly highest breast ca risk.
4. Not breastfeeding :
Some studies suggests that breastfeeding may slightly lower breast cancer risk.An explanation for this possible effect may be that breastfeeding reduces woman’s total number of lifetime menstrual cycle.
5. Birth control pills :
Women using oral contraceptive pills have a slightly higher risk of breast cancer than the woman who has never used them. Risk comes down after stopping the pills.
6. Hormone Therapy after menopause :
Hormone therapy with estrogen that is HRT is usually given to realive symptoms of menopause and to help prevent osteoporosis.
Use of HRT after menopause increases the risk of breast cancer. This increase in risk can be seen with as early as 2 yrs of use. The risk-return to the general level within 5 yrs of stopping treatment.
7. Alcohol Consumption :
Drinking alcohol is associated with the increased risk of breast cancer. The risk increase with the amount of alcohol consumed. Those who have 2-3 drinks/day have about 20 % higher risk compared to women who don’t drink alcohol. Excessive alcohol consumption also increases risk of other cancers too.
8. Diet & vitamin :
High fat diet can lead to being over weight or obesity which is a known breast cancer risk factor. A diet high in fat is also a risk factor for other types of cancer & high risk of heart disease. A diet low in fat, low in red meat & processed meat, high in fruits & vegetables has health benefit.
9. Chemicals in the Environment :
Exposure to chemicals like pesticide insecticides, plastics, certain, aromatic causes higher risk of developing any cancer.
10. Smoking :
Exposure to tobacco & smoking increases chances of getting many types of cancers.
Disproven Factors –
Antiperspirants , bras , breast implants.
Some risk factors are beyond your control like being female and getting older. But the key to reduce risk of breast cancer is to maintain a healthy weight and regular physical excersice. Doing regular physical excersice 4 to 5 hours per week ( 50 mins per day ) will help to maintain normal weight. Avoiding obesity is most important thing. Adapting a good and healthy life style is a key for preventing breast cancer.
For all Woman-
Stay at a healthy weight throughout your life.and avoid excessive weight gain by balancing your food intake with physical activity. Avoid alcohol and smoke.
For women of incresed risk of Breast cancer
This risk is usually determined by a risk assessment tool called cancer model for women with increased risk of breast cancer.
(For eg. women with strong family risk of breast cancer, history of DCIS , LCSS ) can lower the chances of getting breast cancer by following methods –
1) Medicines to lower breast cancer risk.
Tamoxifen in premenopausal women & Raloxifen and aromatase inhibitors in post menopausal women can be used to lower the risk. However these medicines can have side effects so it is important to assess the positive benefits and risk of taking medicines.
2) Preventive surgery
For a small numbers of women who have extremely high risk for breast cancer , surgery of removal of breast may be an option.
For women at increased breast cancer risk who dont want to take medicine or have surgery can be managed with active surveillance and close observation. This helps to find it early when it is likely to be easier to treat.

Diagnosis
The diagnosis of breast cancer is done by Triple Test. It includes 3 things
1) Clinical Examination :
In which the doctor looks for any lump in the breast , nipple discharge , lymph node enlargement and signs of any distant organ involvement.
2) Mammography :
Is done to see for the lump in the breast , wheather single or multiple & any microcalcification (DCIS). It also helps to confirm that the opposite breast is normal [ Sometimes breast cancer can be bilateral i.e in both breasts ]
3) Biopsy :
It includes taking out a small piece from the lump in the breast & examining it under microscope for pathological confirmation . This confirms that the patient has breast cancer.
Mammography
Mammogram is an X-ray of the breast that looks for the changes that may be signs of breast cancer. It can often find or detect breast cancer early, when it is small & even before a lump is felt.
Types of Mammogram
1) Screening Mammogram :
It is used to look for signs of breast cancer in women who do not have any breast complaints or symptoms. X-ray pictures of each breast are taken from 2 different angels.
2) Diagnostic Mammogram :
It is done in women who already have any breast complaints like lump in breast . or if a change is seen or a screening Mammogram , They may include extra view (images), sometimes it is used to screen women which are already treated for breast cancer in the past.
How do Mammogram Work ?
A Mammogram uses a machine designed to look only at breast tissue. The machine takes X-ray of lower dose than usual X-ray. The machine has 2 plates that compress or flatten the breast to spread the tissue apart. This gives better picture & allows less radiation to be used.
A newer type of Mammogram is known as breast tomosysnthesis or 3 D Mammography. For this the breast is compressed once & machine takes many low dose X-ray as it moves over breast. A computer then puts the images together into a 3 dimensional picture. In some cases this uses more radiation than standard 2-view mammogram, but it allow doctors to see breast tissue more clearly.
Are mammogram safe ?
The total dose of radiation used for a typical mammogram is 0.4 mSv [miliSierverts] which is very low . The benifits of mammography out weigh any possible harm from the radiation expose. If a lady is pregnent she should inform before doing mammogram though the risk to fetus is likely very small.
What does doctor look for on a mammogram ?
A radiologist will report a mammogram. Most comman features seen in a mammogram of a patient with breast cancer are 1) calcification 2) Masses or lumps or other signs like area of architectural distortion , spiculated mass.
Calcification :
Are tiny calcium deports within the breast tissue. They look like small white spots on a mammogram. They may or may not be caused by cancer- There are 2 types of calcification.
1)Macrocalcification : They are larger calcium deposits that are due to change caused by aging of the breast arteries or old injuries , inflamation. They do not need to be checked with the biopsy . They are more comman as women get older(75 years)
2)microcalcification : are tiny specks of calcium in the breast. They are more of a concern than macrocalcification. But they dont always mean that cancer is present. The shape & layout of microcalcification help the radiologist to judge that the change is due to cancer.
Mass
A mass is the same as a lump or a tumor. It can be with out calcification . They can be many things like cysts [non cancer fluid filed sacs] , non cancerous solid tumors [fibroadenoma]. But they may also be sign of cancer.
Simple cysts are non cancer & don’t need biopsy . A cysy & a solid tumor look same on mammogram. Sonography (breast ultrasound) can differentiate between cyst & solid tumor. So many times mammography is combined with sonography which is called sonomammography . The size, shape & margin (edge) of the mass helps the radiologist to decide how likely it is to be cancer.
Breast Density
Mammogram gives assessment of breast density . Breast density is based on how fibrous & glandular tisues are distributed in the breast as opposed to fatty tissue. Dense breasts are not abnormal but they are linked to a higher risk of breast cancer. It make it harder to find a lesion on a mammogram.
Limitation of Mammogram
Mammograms are the best breast cancer screening tests we have at this time. But mammogram have their on limits. For example they are not 100% accurate in showing if a women has breast cancer.
i) A false negative mammogram looks normal even though breast cancer is present
ii) A false positive mammogram looks abnormal even though there is no cancer in the breast
iii) Women with dense breast have more false negative results
iv) The odds of a false-positive finding are highest for the first mammogram
v) Women who have earlier mammogram available for comparison reduce false positioning by about 50%
Breast Biopsy
When the clinical examination and sonography or mammography shows abnormal findings like a lump or microcalification in the breast patient will need to have a biopsy. All biopsy results are not cancer , but a biopsy is the only way to find out. In a biopsy the cells from the suspicious area are removed & examined under microscope in the lab to see if cancer cells are present.
There are different types of biopsies. It can be either needly biopsy or surgical biopsy.
Types of Biopsies
1) Fine needle Aspiration Cytology [FNAC]
2) Core Needle Biopsy
- Routine Core Biopsy
- Special types of core biopsies
Stercotactic core needle biopsy
Vaccum-assited core biopsy
3) Surgical Biopsy Two types
I) Incisional biopsy
II) Excisional biopsy
Most commonly done is the core needle biopsy.
Core Needle Biopsy
A core biopsy is a outpatient procedure done under local anaesthesia (Patient is awake but the skin over breast is numbed). Usually it is a quick procedure but if imaging tests are needed or if the special types of CNB described below is used , it may take more time.
In the core biopsy the doctor uses a wide , hollow needle to take out piece of breast tissue from the suspicious area that doctor has felt or seen on imaging tests . A small core (piece )of tissue is taken out in the needle. Several cores are removed.
If the lump is palpable the doctor puts the core needle by feeling the lump. But if the abnormal area is not palpable the needle is put using some type of imaging test to guide the needle into the right place. These imaging test can be either ultrasound (USL), MRI or Mammogram.
Once the tissue (cores) are removed the needle is taken out . Sterile dressing is put . These cores are examined by the specialised doctor that is pathologist in the lab to see for any cancer cells.
Special types of CNB
Stereotactic CNB
This is offten used to biopsy suspicious microcalcifications or small tumeros that can’t be clearly seen on ultrasound . In this procedure mammogram picture are taken from different angles to pinpoint the biopsy site. A computer analyzes the x-rays of the breast & shows exactly where the needle tip needs to go in the abnormal area.
Vaccum Assisted CNB
In this procedure a hollow probe is put through a small cut into the abnormal area of breast tissue using an imaging test. A core of tissue is then suctioned into the probe & a rotating knife inside the probe cuts the tissue samples. This method removes more tissue than a regular core biopsy needle.
Results of CNB
A Pathologist will look at the biopsy tissue to find out it there are cancer cells in it . A CNB is likely to clearly show if cancer is present , but it can still miss some cancers.A Pathologist will look at the biopsy tissue to find out if there are cancer cells in it . If the results of CNB do not give a clear diagnosis or if the doctor still has concern, Patient might need to have a second biopsy or a different types of biopsy.
Surgical Breast Biopsy
In some situations such as if the results of CNB are not clear Patient needs surgical (open) biopsy. For this type of biopsy surgery is used to remove all or part of a lump so that it can be checked to see for cancer cells in it.
There are 2 types of surgical biopsies
- An incisional biopsy – It remove only part of the lump for checking.
- An Excisional biopsy – It remove entire lump or abnormal area.
Wire localization to guide surgical biopsy
[Steriostatic wire Localisation]
If the abnormal area is not palpable(Can’t be felt or hard to find), a mammogram, ultrasound or MRI may be used to place a wire in the suspicious area to guide the surgeon the right spot.
Under local anesthesia this wire is put through a hollow needle and a smooth hook at the end of the wire keeps it in place. The surgeon uses the wire as a guide to the area to be removed.
The pathologist will look, at the biopsy tissue under a microscope to find out if there are cancer cells in it.
Different types of breast cancer
There are many type of breast cancer. Some are more common than others. Some of the most common types of cancer are as follows –
Ductal Carcinoma in situ (DCIS)- This is most common type of noninvasive breast cancer. This type of cancer has not invaded surrounding tissues and has not spread to distant organs. So usually it has a very high cure rate.
Invasive Ductal cancer – It is the most common type of breast cancer. About 80% invasive breast cancer are invasive ductal carcinomas(IDC). It starts in a duct of the breast and grows into the surrounding tissue.
Invasive Lobular cancer – It starts In the glands of the breast .Approximately 10% of invasive breast cancer are invasive lobular cancer [ILC].
The remainder of breast cancer are much less common and include following:
Mucinous ca – formed from mucin producing cancer cells.
Medulary Carcinoma – It is an infiltrating breast cancer that present with cell defined boundries between the cancer and noncancer tissue.
Inflammatory breast cancer – In this type the skin over the breast appear red and feel warm (inflamed).It simulates breast infection that is mastitis. It can also occur in pregnancy.
Triple negative breast cancer – This is a subtype of invasive cancer with cells that lack oestrogen and progesterone receptors and have no excess of specific protein (HER 2) on their surface. It tends to appear more often in younger women and tend to be more aggressive type of cancer.
Pagets disease of the nipple – This cancer starts in the ducts of the breast and spreads to the nipple and the area surrounding the nipple. It usually presents with crusting and redness around the nipple. It may or may not be associated in the lump in the breast.
Adenoid cystic carcinoma – These cancers have both glandular and cyrtic features. They tend not to spread aggressively and have a good prognosive
Lobular carcinoma in situ – This is not cancer but an area of abnormal cell growth that can lead to invasive breast cancer later in life.
The following are other uncommon types of breast cancer –
- Papillary Carcinoma
- Phylloids tumer (malignent)
- Angiosarcoma
- tubular carcinoma
Breast cancer Stages
After a patient is diagnosed with breast cancer, doctor will try to figure out if it has spread and if so how far. This process is called Staging. The stage of a cancer describes how much cancer is in the body. It helps determines how serious the cancer is and how best to treat it. It also helps about survival Statistics. As a rule lower the stage is, the less the cancer has spread. A higher the stage such as stage IV means cancer has spread more.
The staging system most often used for breast cancer is the American joint committee. It has both clinical and pathological staging on cancer (AJCC) TNM systems. It takes into account many parameters like tumors(T) spread to nearby lymph nodes(N), spread to distant organs(M): Pathological staging also gives informative regarding Estrogen Receptors[ER] status, progesterous Receptor[PR] status, Her2/new[HER2] status and grade of the cancer.
Stage 0 – Known as ductal carcinoma in situ (DCIS) or Lobular carcinoma in situ (LCIS) .The cells are limited to within a duct or lobular . The cancer cells have not invaded the surrounding tissues.
Stage I – The tumor is about 2 cm across and it has not spread to any lymph nodes.
Stage II – The tumor as about 2-5 cm across and may have spread to nearby lymph nodes.
Stage III – The tumor is more than 5 cm and may have invaded to the skin or underlying muscle and spread to lymph node.
Stage IV – The tumor is not limited to breast only and spread to distant organs of the body like bones, lung, liver or brain.
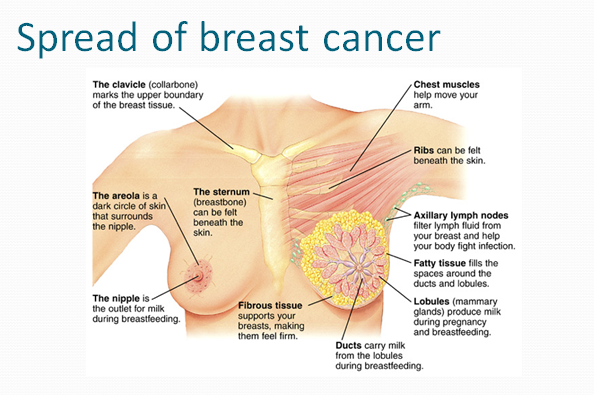
Spread Of Breast Cancer
Breast cancer can spread to surrounding tissues by local Invasive or to the distant organs of the body through blood or lymph spread.
1)Local Spread
Breast Cancer Can invade surrounding tissues like underlying muscle or rib or overlying skin on the skin of breast.
2) Lymphtic Spread
By lymphtic vessels carying lumph from the breast to the lymph nodes cancer can spread to nearby lymph nodes. Most commonly it spread to axillay lymph nodes ,but it spread to internal mamary or supraclavicular lymph node.
3)Blood spread
Through blood cancer can spread to distant organs .In breast cancer most commonly it may spread to bones,lugs,liver or brain .When spread to other organs,patient develop complain like bone pain,fracture,jaundice or cough.
Treatment Of Breast Cancer
Treatment of breast cancer is called multi modality treatment because it includes different ways of treatment . Treatment of breast cancer is given by a team of specialist which include a breast surgeon ,Oncophysicion ,a radiation Oncologist ,Physiotherapist & a Counselor.
Total treatment include Following things:
1)Surgery
2)Chemotherapy
3) Radiation Therapy
4)Harmonal Therapy
5)Targeted drug Therapy
A breast cancer patient usually need all type of treatment but in selected cases patient may need one or four types of treatment.It depends on stage of tumor ,type of tumor & individual preferences.
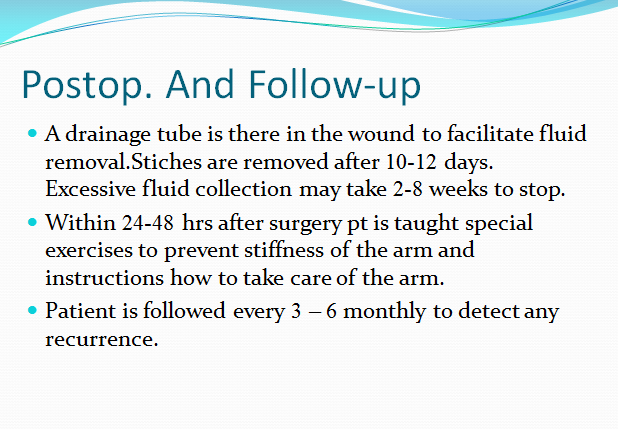
Surgery for Breast Cancer
Type of surgery for breast cancer treatment depends upon the stage of disease & individual Preference.
1)Mastectomy[MRM] .
Removing total breast cancer that is removing all the robules,ducts,fatty tissue,skin overlying the breast and all the lymph nodes and fat in axillary area.If immediate reconstruction is considered, skin sparing mastectomy is sometimes preferred . In this all the breast tissue is removed but the overlying skin is preserved.
2)Breast conservation surgery[BCS]
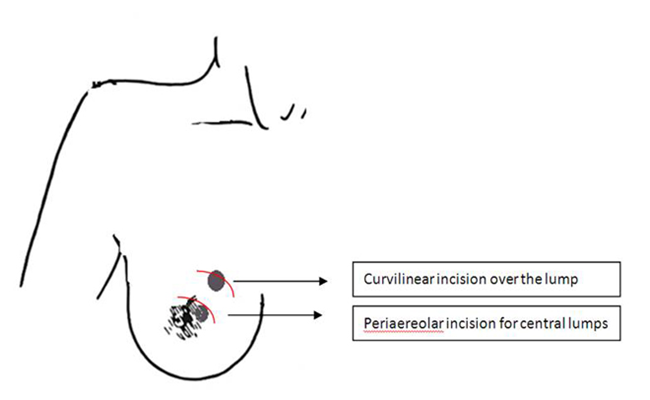
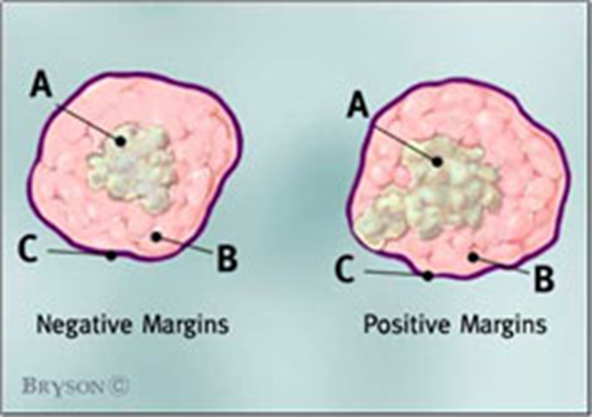
It includes lumpectomy & axillary dissection. Lympectomy is removing the tumor and a small margin of surrounding normal tissue. The extent of surgery is determined by the size & location of tumour .The margin of the lumpectomy specimen are examined by the pathalogist for cancer cell whether cancer cells are found at the margin of lumpectomy specimen. Then patient may need other procedure that is revision of margin of lumpectomy. BCS is always followed by radiation therapy.
3) sentinel node biopsy
In few early detected cases of breast cancer removing all lymph node in armpit [axillary dissection]may not be needed. In such patient removing the specific lymph node is [sentinelnode] may be sufficient to stop the cancer spreading.
4)Reconstruction
Reconstruction surgery is done for cosmetic purpose .After breast cancer surgery Reconstruction surgery can recreate the breast so that it looks similar to the other breast.This can be done at the same time of primary surgery or at later date. The surgeon may use a breast implant or tissue from another part of the patient body.
5) Preventive Surgery
In a small number of patients who have extremely high risk of developing breast cancer ,surgery to remove the breast may be an option. This prophylactic (preventive ) surgery can decrease the risk of breast cancer by 90% for women at moderate to high risk of breast caner. This should be thoroughly discussed including , genetic testing for BRCA-1 or BRCA-2 mutatuion , risk factors , family history and other preventive options like medications.
Chemotherapy
Chemotherapy is giving anticancer medication (cytotoxic drugs) either by intravenous injection or by mouth. Chemotherapy can be given in different settings as follows –
1) Adjuvant Chemotherapy
It is given after surgery to destroy the possibility of cancer cells spread. In a very small number of patients with very low risk of recurrance Chemotherapy can be avoided.
2) Neoadjuvant Chemotherapy
If the tumor is large , Chemotherapy can be given before surgery to shrink the size of tumor and to make its removal earlier .
3) Chemotherapy
For advanced cancer If the cancer has spread to other parts of the body Chemotherapy can be given to reduce symptoms. There are many Chemotherapetic drugs which can be given alone or usally in combination. They are given usually in cycle with certain treatment intervals followed by a rest period. The cycle length and rest interval differ from drug to drug . The side effects of Chemotherapy include nausea, vomiting , loss of appetite, fatigue, sore mouth , hair loss and more suscephibility to infection. Medication are usually given to help control the side effects.
Radiation Therapy
Radtion therapy is giving a controlled doses of radiation (high energy rays ) at the tumor to destroy the cancer cells. It can be administred by two ways.
1) Enternal beam radiation
This is the usual way of giving radiation theropy to breasts cancer patients . A beam of radiation is focussed on the area by an external machine. The treatment is given five days a week for five to six weeks Adverse effects include fatigue, lymphodema , darkning & irritation of the breast skin.
2) Brachy Therapy
In this radiation therapy delivered by using radioactive seeds that are implanted into breast tissue.
HarmoneTherapy
Harmone therapy blocking therapy is used to prevent recurrence in harmone sensitive breast cancer. These tumors are called ER psitive (Estrogen recepter) & PR positive (Progesterone receptor) cancers. Usually they are started after surgery & chemotherapy. But they may be given earlier. It may be the only option for patients who cannot undergo surgery, chemotherapy or radio therapy. The effect normally last for upto 5 years after surgery. This treatment has no effects on cancers that are not sensitive to hormones. So this treatment is not given in tumor receptor negative tumors patients. Examples are Tamoxifen – This drug prevents estrogen from binding to breast cancer cells Aromatase inhibitor – They stop estrogen production in postmenopausal women. Ovarian ablation or suppression – either by drugs (LHRH agonist drug called goseretin) or radiation or by surgery. Harmone treatment may affect a women future fertility.
Targeted Therapy
Targeted drugs destroys specific types of breast cancer . Examples are transtuzumab (herceptine), lapatinib , Bevacizunab.They are used in HER-2 positive tumors. They may be used after chemotherapy or alone.